If you’ve suffered a heart attack, a critical “survivor’s step” you should take is to increase your Omega-3 Index.
This is one of the findings of a new study that examined the long-term health outcomes of patients following a heart attack.
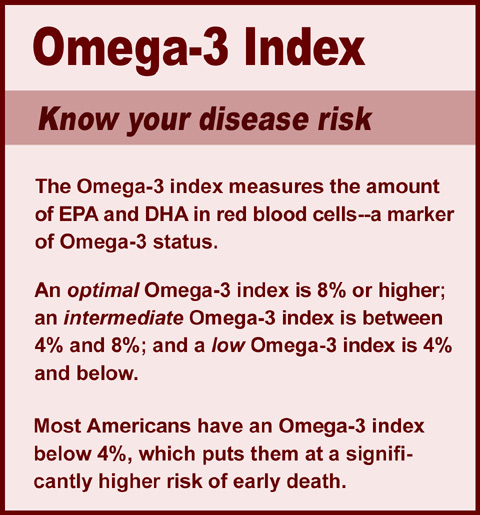
The Omega-3 Index refers to a measurement that assesses the levels of Omega-3 fatty acids, specifically eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), in the red blood cells.
It is expressed as a percentage and serves as a valuable indicator of one’s overall cardiovascular health.
An individual’s Omega-3 Index status can also provide insight into risk of other diseases and can help healthcare professionals make informed decisions regarding dietary recommendations and supplementation.
People can improve their Omega-3 Index by consuming high Omega-3 foods—such as fish, flax seeds, seaweed, alage and walnuts—or by taking a quality nutritional supplement.
Omega-3 fatty acids are considered “essential nutrients” since they play a crucial role in various bodily functions, and the human body cannot create it. Omega-3s are recognized for their anti-inflammatory properties. Numerous studies have linked Omega-3s to a reduction in chronic diseases such as diabetes, heart disease and certain types of cancer.
The new research, published in the International Journal of Cardiology, assessed what happened to participants over an average period of 6.5 years following a myocardial infarction.
“Even after two years the number of cardiac events was way lower in those who had been treated with Omega-3 for just six months. That’s a very impressive finding,” said author on the paper William S. Harris, PhD, professor of internal medicine at Sanford School of Medicine, University of South Dakota.
Harris is also president of the Fatty Acid Research Institute and founder of OmegaQuant Analytics, the organization that developed the Omega-3 Index.
Study details
Researchers recruited 360 patients who had experienced heart attacks were subsequently admitted to hospitals in the Boston area. Participants were divided into two groups: experimental and placebo.
Participants in the experimental group received 4 grams daily of an Omega-3 supplement provided by a national brand. Each Omega-3 fatty acid capsule contained both EPA and DHA.
Prior to treatment, researchers measured baseline red blood cell fatty acid levels, serum lipids and insulin resistance markers. Cardiac magnetic resonance studies were also conducted on the patients at baseline and following the six months of initial study treatment.
Participants were then tracked for an average time of 6.6 years. (The shortest observation was 5.0 years while the longest was 9.1 years). The scientists then assessed whether there was a difference in the rate of major adverse cardiac events between the two groups. They also determined whether the participants had experienced at least a 5% increase in the Omega-3 Index while they were on treatment.
Researchers followed the patients at two-month intervals using scripted telephone interviews, or by questionnaires via mail, during the six-month treatment period. When the treatment was completed, another outpatient visit was scheduled, and blood sampling and cardiac magnetic resonance were repeated. Afterward, patients were followed every six months for three years, then yearly.
Researchers found patients who were treated with Omega-3 fatty acid supplements and achieved a 5% rise in Omega-3 Index experienced a significant reduction of adverse cardiac events after a median follow up period of 6.6 years.
The researchers chose a cutoff of a 5% increase of the Omega-3 Index as this change was associated with a lower rate of cardiac arrest in a prior study.
Most of the population is Omega-3 deficient
While the U.S. government still has not established an official recommended daily allowance for Omega-3s, the U.S. Department of Agriculture’s Dietary Guidelines for Americans does recommend that people eat at least two servings of fish per week to maintain adequate Omega-3 blood serum.
Most Americans do not meet even this meager guideline; moreover, vegetarian consumers typically do even worse since they don’t consume the rare plant foods that contain both DHA and EPA Omega-3s—such as algae and seaweed.
In a study published in May 2021, researchers analyzed two years of U.S. population data from the National Health and Nutrition Examination Survey (NHANES) and determined that over 68% of adults and 95% of children in the United States did not consume enough Omega-3s to meet nutritional standards.
These widespread deficiencies might have played a part in the current study as some of the test group did not see an increase in their Omega-3 Index even with supplementing. This could be due to deficiencies being so excessive that a more aggressive intervention is necessary—such as a period of supplementing longer than six months.
“I want people to realize that achieving a healthy blood level of Omega-3 is not automatic if you’re taking an Omega-3 supplement or drug (as in this study),” Dr. Harris said. “Achieving the optimal blood level is the primary goal, not just taking the pills.”
– – –
All three Omega-3 essential fatty acids can be found in Optimal E.F.A. by Optimal Health Systems:
• A-linolenic acid (ALA)
• Eicosapentaenoic acid (EPA)
• Docosahexaenoic acid (DHA)
Click the banner ad on this page, or visit the product info page here.
– – –
Source: International Journal of Cardiology.