Your mom knew fruit and vegetables were good for you, but she probably didn’t know they were critical for fighting one of today’s most prevalent health conditions: allergies.
Researchers at Tokyo University of Science have discovered (or some may say, rediscovered) a vital connection between dietary fibers, gut health, and the immune system.
Dietary fibers are found in fruits, vegetables, legumes, nuts and grains.
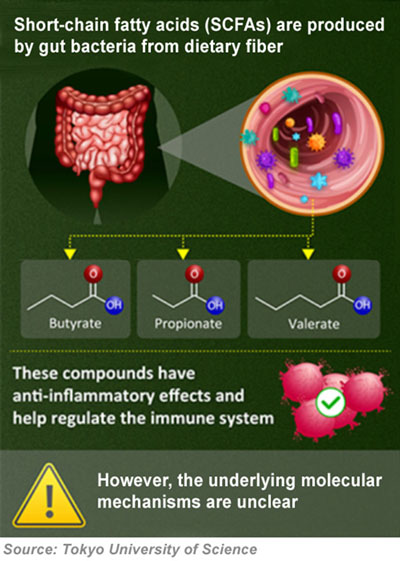
The study showed that a vital health benefit was provided by the short-chain fatty acids (SCFAs) that are produced in the gut by dietary fiber and gut bacteria.
According to the researchers, the complex biological relationship between gut bacteria and critical fiber provides a “significant anti-inflammatory and immunomodulatory effect.”
Allergy rates soaring worldwide
If you think allergies are more common now than a few years ago, you’re not wrong. Estimates are that 30 to 40% of the world’s population now have some form of allergy.
According to health professionals who specialize in allergies, allergic reactions—everything from hay fever to eczema and asthma—have skyrocketed around the world in the last few decades.
The reasons for the rise are often debated; however, there is some common ground.
In her new book, Theresa MacPhail, an associate professor of science and technology studies at Stevens Institute of Technology, sums up some of the main reasons in her new book, Allergic: Our Irritated Bodies in a Changing World:
• An excessive emphasis on hygiene (perhaps even over-showering) contributes to the development of sensitivities.
• A rise in exposure to environmental toxins, which reduces the skin’s ability to ward off potential allergens.
• A shift in our diets over the years toward more processed foods and less health-protecting fiber.
The shift in diet as a cause of allergy increase is certainly in line with the findings of the new Japanese study. The fiber received from a regular intake of fruit and other high fiber foods is critical to many aspects of health—including for building and maintaining the immune system.
According to the Tokyo University of Science researchers, SCFAs, found in plant-based foods, are metabolized by gut bacteria, leading to the production of molecules with potent effects on the body’s immune system.
The focus of their research was on how these SCFAs influence mast cells, a type of white blood cell integral to allergic responses. Mast cells release histamine and other substances upon detecting foreign bodies, which can cause allergic reactions.
The Tokyo University of Science’s study—actually, a series of experiments—demonstrated that two specific SCFAs, butyric acid and valeric acid, were able to suppress allergic reactions in mice.
Study findings
The study further explored this effect in mast cell cultures, showing that SCFAs could prevent the activation of these cells—the process that typically leads to allergies.
The mechanisms demonstrated in the experiments suggests that SCFAs can significantly reduce allergic responses, highlighting the importance of dietary fibers in managing allergies.
The study also found that the use of non-steroidal anti-inflammatory drugs (NSAIDs) can negate the beneficial effects of SCFAs. This adds still one more reason for the growing rates of allergies, since NSAIDs are so widely used today.
“The activation of mast cell is a common cause of various allergic diseases and not limited to anaphylaxis,” says study lead author Chiharu Nishiyama, professor at Tokyo University of Science, in a university release. “In addition, I think that the increasing frequency of allergic patients is associated with changes in diet in these decades.”
The research underscores the complex interplay between diet, gut microbiota, and immune system regulation.
Unfortunately, although studies like this provide a scientific basis for dietary recommendations aimed at preventing allergies, the world’s medical establishments are wholly invested in allopathic-pharmaceutical medicine, not hollistic medicine. This means it is an almost impossible task to convince decision makers to move away from drug interventions in favor of promoting diet interventions.
But Nishiyama and his team appear to be undeterred by the roadblocks.
According to the university press release, they hope by focusing future studies on the relationship between “specific SCFAs and the mucosal environment” they will uncover further health benefits of various foods. They hope this will potentially lead to improved dietary guidelines and healthier lives.
“It is important to demonstrate with scientific evidence how dietary conditions affect health,” Nishiyama concluded.
In addition to the university press release, the complete study was published in The Journal Of Immunology in January 2024.
– – –
Sources: The Journal of Immunology, Tokyo University of Science.