For anyone who has done even a modest amount of research on Vitamin D, the censorship of any discussion on the nutrient relative to Covid is baffling.
After all, Vitamin D has been recognized as a critical nutrient for humans for a century—and specifically as a critical nutrient for immune function for half a century.
So why wouldn’t it be an important part of the discussion when it comes to Covid-19?
Vitamin D regulates the expression of thousands of genes in the human body via its interaction with specialized cellular proteins called “Vitamin D receptors.”
Nearly all cell types involved in the body’s immune response possess Vitamin D receptors. These cell types include monocytes/macrophages, T cells, B cells, natural killer cells, and dendritic cells.
Consequently, Vitamin D plays essential roles in the regulation of both innate and adaptive immune systems.
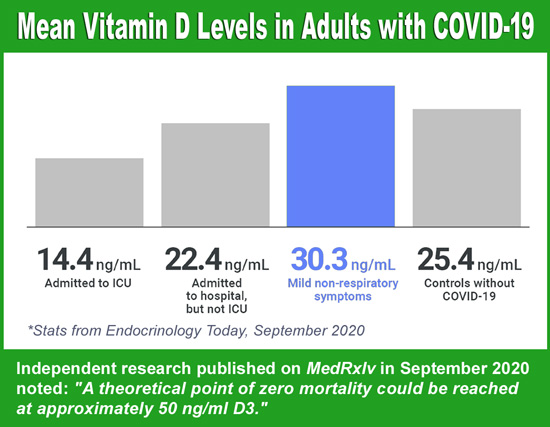
If Vitamin D is so critical, then what is an optimal level to have in one’s blood? The Endocrine Society defines optimal blood levels of Vitamin D as 40 to 60 nanograms per milliliter (ng/mL).
Unfortunately, based on Endocrine Society standards, about 40 percent of people living in the United States are deficient in Vitamin D. Certain populations are at greater risk for deficiency, especially older adults, dark-skinned people, and people who are obese or have diabetes.
Long before the Covid era, deficiency was associated with numerous health conditions: poor bone health, higher cancer risk, higher risk of depression, higher incidence of seasonal flu, and even shorter lifespan overall.
So, it is not surprising that evidence—supported by independent studies from more than 20 countries—also points to high Vitamin D deficiency rates exacerbating the Covid-19 pandemic.
In fact, it was obvious that Vitamin D—and Vitamin D3 specifically—was playing a pivotal role in the pandemic. Asian countries, where there is less censorship on the subject, were the first to publish findings that Covid outcomes were worse for D-deficient Covid patients.
After the connection was made, however, there was much debate regarding whether low Vitamin D3 was caused by the infection, or if having a deficiency at onset resulted in a worse outcome.
To help settle the debate researchers recently analyzed data from one population-based study (which measured long-term Vitamin D status in more than 400 million people worldwide) and seven clinical studies (which measured Vitamin D levels post-infection).
Researchers utilized a machine learning model to compute the expected death rates among the patients.
The machine learning was based on characteristics such as the patients’ age, sex, median Vitamin D levels, and whether they had diabetes. The timeframe for the data collection preceded the advent of vaccines against COVID-19, so vaccines played not part in the research.
The analysis revealed that people who had optimal Vitamin D levels preceding SARS-CoV-2 infection were highly unlikely to die from their illness, suggesting that Vitamin D reduces the risk of death from COVID-19.
“The two datasets provide strong evidence that low D3 is a predictor rather than a side effect of the infection,” the authors wrote in their conclusion.
In fact, the results were so profound the researchers theorized that Covid-19 deaths would be virtually eliminated if Vitamin D3 levels could be raised significantly: “COVID-19 mortality risk correlates inversely with Vitamin D3 status, and a mortality rate close to zero could theoretically be achieved at 50 ng/ml,” the researchers wrote in their summary.
The research was published online at MedRxiv in September 2021.
MedRxiv (pronounced “med-archive”) is a free online archive and distribution server for complete but unpublished manuscripts (preprints) in the medical, clinical, and related health sciences. Preprints are preliminary reports of work that have not been certified by peer review.
Vitamin D is included in a number of popular Optimal Health Systems products. Follow links below for more information:
• Essential DAK1K2
• Exposure Protection Pak
• Optimal Whole Food Vitamin-Mineral
• Optimal Longevi-D
• Opti-Immune-VRL
– – –
Sources: MedRxiv.org, Endocrine.org, Helio Journals.